- Gaps in care
- Suspect conditions
- HCCs
- Provider incentive program performance
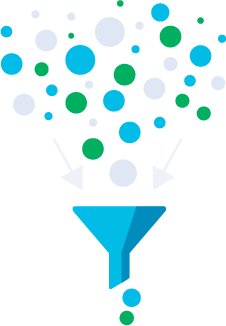
MINIMAL DATA.
MAXIMUM OUTCOMES.
The streamlined platform transforms
massive amounts of data into actionable,
high-impact clinical insights.
BENEFITS
The value-based care accelerator
Everything delivered
right in the EHR
With our fully customized platform, physicians don’t have to go
outside the existing clinical workflow to uncover:
At-a-glance data insights provide better care to patients
With more than 1,400 clinical rules, our platform distills a mountain of patient
data into a strategic, easy-to-scan checklist of the most pressing concerns.
Powerful CDI for the
outpatient setting
Our technology brings the rigor and sophistication of hospital-based CDI
into the physician’s office to deliver groundbreaking prospective risk
adjustment.
Custom-tailored for
better workflows
We customize our platform to each organization we work with to cut
onboarding time and streamline provider workflows.
Quick loop-closing
on reports
No more waiting for a claim to be completed. Our platform delivers clinical activity summaries in just days, not weeks or months.
56%
higher RAF value
$230k
in equivalent MA revenue
generated
Up to $16M
total savings at a single
medical center
9/10
Net Promoter Score
from physicians
OUR FEATURES
Access to curated data that matters
Automated Rules Engine
Our platform analyzes thousands of EHR and claims data points including provider notes, labs, medication, devices, procedures, conditions lists, scanned documents, and national and state HIE.
Pre-Visit Summary
Clinicians get an easily scannable summary of a patient’s health history, including verified care gaps and suspected (but unmanaged) medical conditions.
Patient Brief
The curated patient brief gives providers actionable insights at the point of care, right in the EHR. It can even be configured to deliver on tight turnarounds, even same-day appointments.
Advanced Diagnostic Tools
With automated tools like configurable static BPA and diagnosis preference lists, our platform streamlines a physician’s updating process.
Post-Visit & Pre-Claim Review
Our prospective reports confirm a patient was given clinically appropriate and compliant care by the provider to reduce RADV audit risk.
Enhanced Queries
When needed, the HCC coder will query the provider via their EHR to get more info and documentation.
OUR PROCESS
How it works

Patient
schedules visit

The platform generates a
rich brief of any care
gaps and suspect
conditions
Select cases are triaged to a
pre-visit reviewer based on
complexity and staff capacity
Physician reviews curated
content with the patient
at the point of care
Physician documents
conditions addressed
Coder queries provider, if
necessary, for clarification or
next steps prior to finalizing bill

When finalized, bill is sent.
Providers
You want to spend time with your patients, not deciphering the thousands of data points your current system throws at you. Only Curation Health, a Reveleer company, delivers the highest-value insights exactly when you need them, right in your current EHR.
Health Plans
To deliver on your promise of value-based care, you need both a roadmap and the vehicle to get you there. Curation Health, a Reveleer company, has built an outpatient CDI platform that acts as the infrastructure for your VBC initiatives, while supporting clinicians in their decision-making at the point of care.