Pilot Study with AdventHealth Reveals an Innovative Use of AI to Decrease Labor Costs, Increase Overall Efficiency in Value-Based Analytics, Workflow, Documentation and Coding
Shortage of Coding and Documentation Integrity (CDI) Professionals Raises the Urgency of Identifying New Ways to Leverage AI
Nearly half of all health care reimbursement currently flows through shared savings, shared risk, bundled payment, population-based payments, or integrated finance and delivery system payments. Government programs specifically use the hierarchical condition category (HCC) risk-adjustment (RAF) model to appropriately pay insurers and providers based on the illness burden of the population served.
To comply with the Center for Medicare and Medicaid Services (CMS), provider organizations continue to make major investments in systems and processes to ensure physicians are correct and thorough in their risk-based documentation, coding, and management of pertinent patient conditions. Many of these support systems entail a blend of information technology and dedicated human coding and documentation integrity (CDI) professionals. Due to the national health care workforce shortage, CDI professionals are increasingly more difficult to find and resulting labor costs are escalating placing undo stress are provider budgets. It is becoming increasingly urgent to identify new and better ways to leverage technology. The healthcare industry must find ways to ensure human professionals work efficiently and at the top of their clinical license.
AdventHealth, Facing Shortage and Prohibitive Cost of Clinical Documentation and Integrity (CDI) Professionals, Engages with Partner Curation Health to Test Expanded Use of AI In Risk-Based Analytics and Workflow
AdventHealth is headquartered in Florida, with 8,200 beds, 1,200 outpatient locations, and manages over 650,000 lives under risk contracts. AdventHealth partners with service and technology services provider Curation Health for value-based care analytics, documentation, coding, and care team information support.
In the spring of 2022, AdventHealth experienced a major personnel shortfall and operational direct-cost overruns related to the scarcity of coding and documentation improvement (CDI) professionals. Curation Health was in the process of redesigning its current Platform to continue to provide highly accurate information with the use of fewer CDI professionals. AdventHealth leaders worked with Curation Health to design a pilot that would test a new way of leveraging the artificial intelligence (AI) in the Curation Health Platform. The goal was to determine whether the AI could be used to greater effect–making more efficient use of scarce and costly CDI professional time–without compromising clinical quality, information accuracy, and physician experience with the overall information and workflow support that they receive.
Overview of the Curation Health Platform, As Deployed at AdventHealth
As deployed at AdventHealth, the Curation Health solution consists of three components: (1) A pre-visit analysis of each patient in which the Curation Health Platform sorts through broad sets of data to identify potential clinical conditions to be addressed. This output is then reviewed by CDI nurse professionals for appropriateness and completeness before presentation to the providers. (2) The resulting clinical insights are then available as a visit preview/opportunity summary, integrated into the EMR, at the point of care. In this visit preview step, the Platform flags both existing and potentially new conditions for providers to consider addressing (especially ‘hierarchical category conditions’ or HCCs that put patients at risk of further complications or avoidable admissions). (3) Post-visit services are then conducted to verify clinical documentation correctness and thoroughness. AdventHealth provides a highly trained team of professional coders on the back end to review the documentation provided in each case to ensure documentation and coding integrity prior to the bill being released to the payer.
The general measure of the Curation Health solution’s success is its effectiveness at processing large amounts of data in the electronic medical record, surfacing the most salient information, and then filtering and prioritizing that information to highlight the highest-merit information items for physicians, following the principles of data minimalism.
The Curation Health solution combines technological and human elements in the following way:

The technology solution behind the Curation Health Platform uses artificial intelligence (AI) to process massive amounts of data about the patient and pull forward potentially relevant opportunities.
A team of human clinical documentation integrity (CDI) professionals then helps clean, organize, and winnow the opportunity list down prior to sending to physicians to prepare for the patient visit. The team also supports physicians with additional documentation and compliant queries.
Three Cohorts to Calibrate Right Mix of Technology and CDI Time
To test the efficacy of tightening the evidence threshold in the rules built into the Curation Health Platform, together with maximizing the use of human CDIs, Advent Health and Curation Health designed a four- month experiment. Three workflow cohorts were created.
Cohort 1: ‘Control Group’ (CDIs review all/existing legacy system)

AI surfaced opportunities with moderate to high confidence scores for CDI review; CDIs then reviewed all surfaced opportunities before sending to physicians. This cohort provided a control, using the standard approach of 100% review by CDI Nurse Professionals and the existing Curation Health Platform.
Cohort 2: ‘Tech Only’
AI surfaced evidence for qualifying conditions and prioritized them to high confidence items. These potential opportunities were sent directly to physicians in an annotated (but unfiltered) brief–without CDI review. This cohort used the enhanced version of the Curation Health Platform with no CDI Nurse Professional review on the front-end.
Cohort 3: ‘CDI Select’
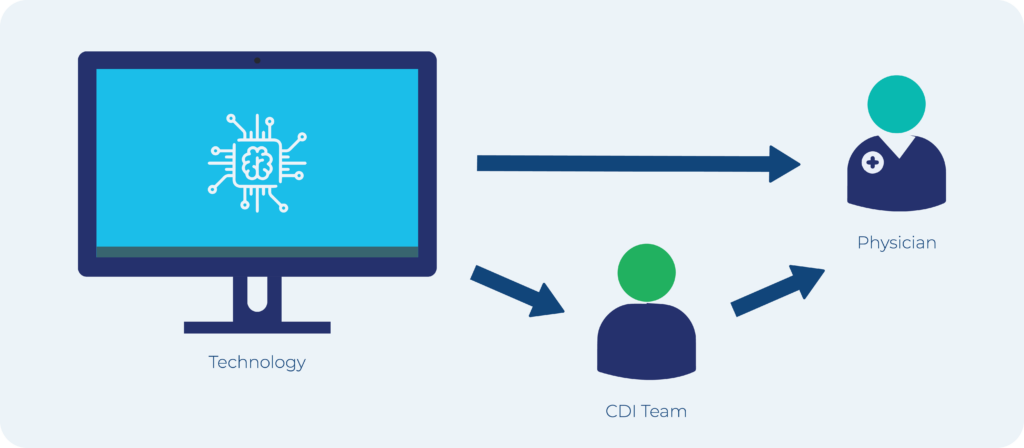
The Platform used AI to surface and send evidence for high-confidence qualifying conditions only and then selectively sent them either to physicians directly or to CDIs for pre-visit review (putting 50% of visits in each category). The briefs on patient visits that the AI determined to be the most straightforward were sent to physicians directly. However, the briefs that the AI determined needed human pre-visit processing were sent for CDI review. In this cohort, CDIs saw fewer (better prioritized) total opportunities than they did in the control group. Thus, this cohort used the enhanced version of the Curation Health Platform and an algorithm to route more difficult cases only to CDI Nurse Professional review on the front-end.
Information Quality, Not (Just) Quantity
In assessing the ‘tech only’ and the ‘CDI select’ cohorts’ performance against the control group, AdventHealth and Curation Health leaders looked primarily at HCC capture, or ‘provider acceptance’ rate. This metric indicates the cleanness and correctness of the information that reaches the physician prior to, or during, the visit. The appropriateness of HCC capture was validated on the back-end through the 100% review by the AdventHealth post-visit review coding team to ensure both under- and over-coding was prevented.
HCC capture rate (or ‘provider acceptance’ rate) tracks the clinical relevance of the opportunity lists sent to physicians–and also to the CDIs, if they are reviewing the record ahead of the visit. It essentially demonstrates how accurate the system is in identifying care gaps by noting the rate at which the potential conditions are confirmed by the physician during the visit and the post-visit review. Strong performance on HCC capture rate indicates that neither CDIs nor physicians are being overwhelmed with long lists of low-merit possibilities–and that care team attention is going to the clinical conditions that are most likely to need active management to support high quality patient outcomes.
‘CDI Select’ Is the Winner
The percentage of HCCs captured per patient was significantly higher in the two cohorts that had tighter prioritization rules in place–and the ‘CDI Select’ cohort (#3), in which the AI in the Platform did selective routing to a human CDI, performed best overall.
Physicians did not report any user-experience issues related to the selective routing approach.
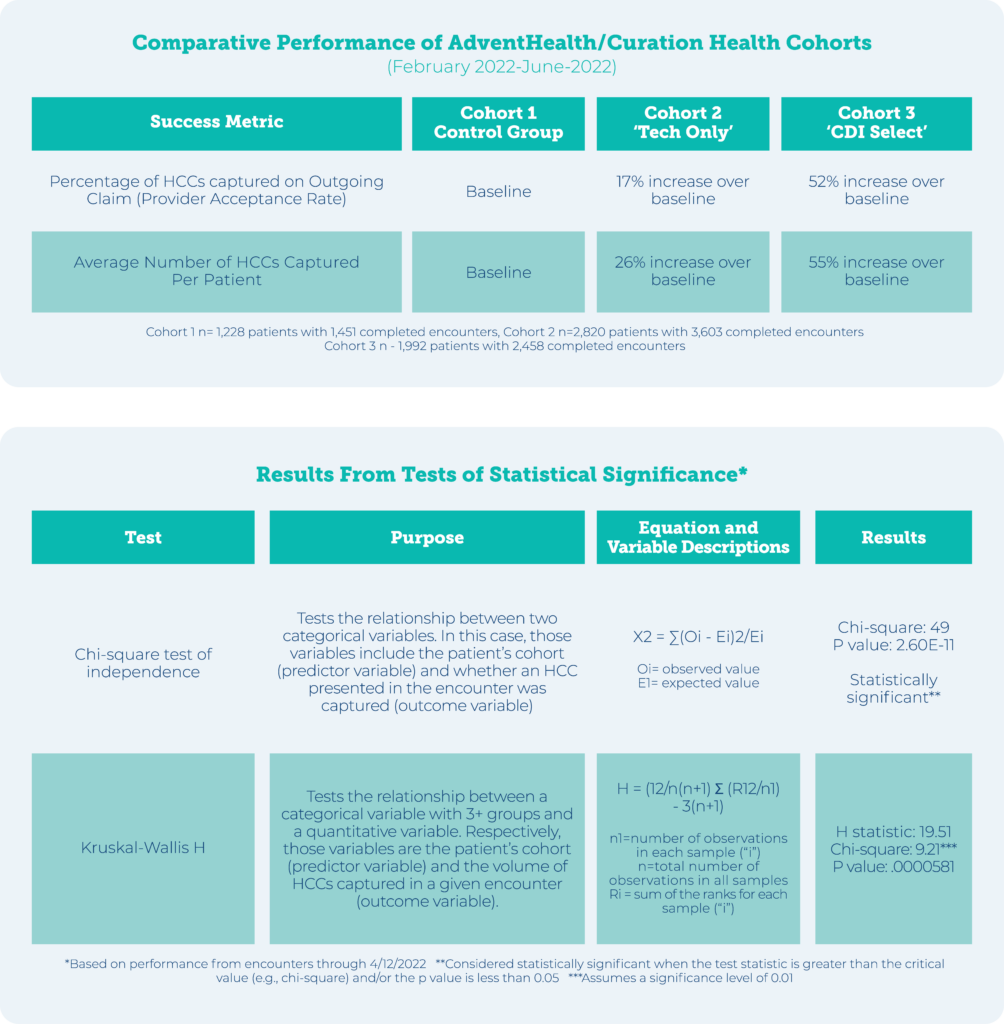
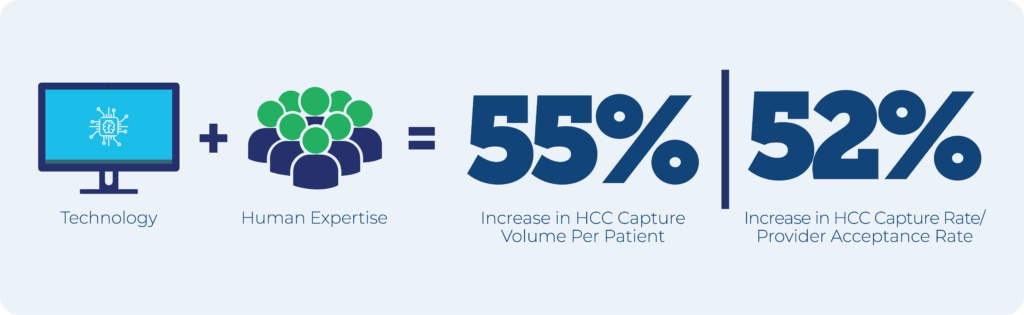
The increase in AdventHealth’s total HCC capture rate was attributed to a more succinct, high-merit-only presentation of information for physicians–which helped prevent legitimate care gap opportunities from accidentally becoming lost in the noise.
“This is about value creation,” said Vice President and Chief Medical Officer Thomas Diller, MD. “What we are getting are better results and, at the same time, we found we were twice as efficient with our CDI Nurse Professional resources.”
“AdventHealth was the first group that was interested in doing this with us. They enabled us to develop this really advanced approach to load balancing,” said Kevin Coloton. “Now that we have identified how we can load-balance pre-visit work, that opens a new world of possibilities for us to serve clients of all sizes and complexity. Because we can tailor our tech to meet their priorities and their existing resources and scale up and down based on their evolving needs.”

