Time to Reflect, Adjust, and Dial Up the Precision
You may know the song about how for everything there is a season. As it turns out, this is absolutely true – including for providers looking to succeed at value-based care (VBC).
Thriving under value-based care requires segmenting the calendar into sprints
VBC contracts–specifically, Medicare Advantage contracts–have an annual pattern. Patients are ‘locked in’ for a calendar year, during which contract-relevant conditions need to be either recaptured, or marked resolved. This, in combination with the natural seasonality in the work calendar and patients’ behavior, means every month of the year deserves a distinct focus in VBC operations.
Entering April, it’s time to reflect, adjust, and dial up operational precision for Q2. With many patients still needing to be brought in for the year, there tends to be little staff capacity for in-depth analysis or strategic plan development, much less rollout. However, with Q1 (and the initial AWV push that came with it) in the books, administrators should have enough “game film” for the year to quickly diagnose and make quick fixes in problem areas. And providers have enough “game time” remaining for the year to realize the benefits from those improvements before the clock runs out.
Key questions administrators should ask:
How are we pacing toward mid-year deadlines for risk adjustment?
Your organization should have data to determine how it is pacing toward reasonable risk adjustment. The key starting ingredient is an informed guess as to what the overall risk of the population should look like, based on prior year and demographic data available from CMS. Compare this number with a current (as of Q2) analysis of what your overall risk adjustment factor looks like – keeping in mind quarter-by-quarter benchmarks that apply to most provider organizations – to determine if you are on track.
Where are the pockets of opportunity?
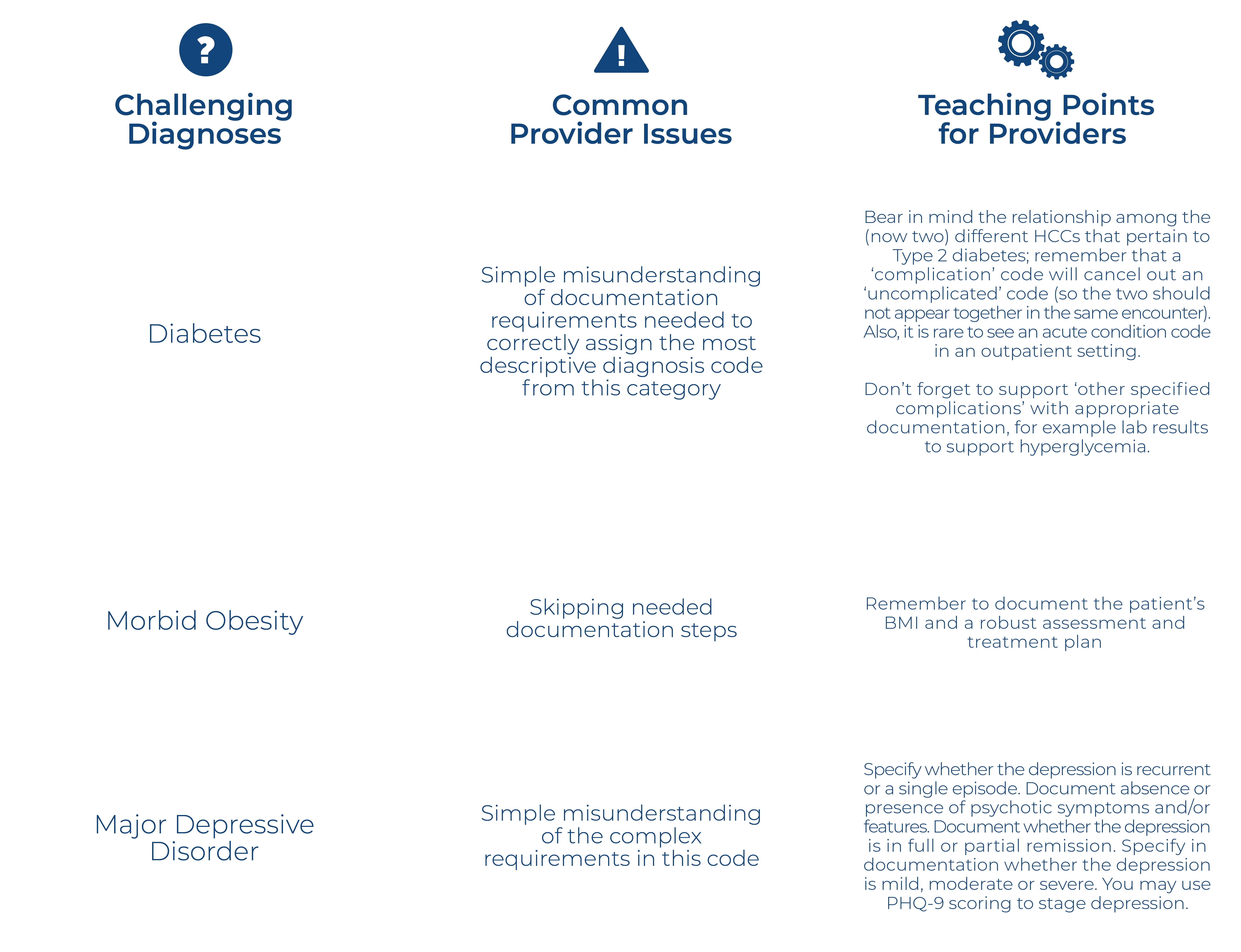
To identify the most promising areas of immediate improvement, run analyses to determine which providers are performing higher vs. lower at thoroughly and accurately documenting conditions. Similarly, analyze which conditions in particular providers are documenting well versus those they are struggling to document.
While major training should be reserved for Q4, once most patients have already been seen and capacity is freed up for strategic initiatives, the right time to do quick interventions to help struggling providers or teams is always ‘right now.’ When major training is enacted, consider taking a peer-led angle to ensure the most impactful training.